How Podiatrists Treat Bunions
 Podiatrists, or foot doctors, can take different approaches to treating bunions, which are structural deformities of the joint at the base of the big toe. This condition not only can cause pain but may also lead to a cascade of secondary foot problems, affecting mobility and quality of life. Initial treatment strategies may include non-invasive interventions aimed at alleviating symptoms and halting the progression of the deformity. Possible strategies include the use of custom orthotics designed to redistribute pressure away from the affected joint, targeted exercises to maintain joint mobility, and advice on appropriate footwear that accommodates the bunion without exacerbating discomfort. In more severe cases, podiatrists may recommend surgical intervention. This surgery, known as a bunionectomy, involves realigning the toe by correcting the abnormal angle of the bones, addressing the issue both cosmetically and functionally. If you have a bunion, it is suggested that you seek the care of a podiatrist who can recommend treatment options to prevent the condition from worsening.
Podiatrists, or foot doctors, can take different approaches to treating bunions, which are structural deformities of the joint at the base of the big toe. This condition not only can cause pain but may also lead to a cascade of secondary foot problems, affecting mobility and quality of life. Initial treatment strategies may include non-invasive interventions aimed at alleviating symptoms and halting the progression of the deformity. Possible strategies include the use of custom orthotics designed to redistribute pressure away from the affected joint, targeted exercises to maintain joint mobility, and advice on appropriate footwear that accommodates the bunion without exacerbating discomfort. In more severe cases, podiatrists may recommend surgical intervention. This surgery, known as a bunionectomy, involves realigning the toe by correcting the abnormal angle of the bones, addressing the issue both cosmetically and functionally. If you have a bunion, it is suggested that you seek the care of a podiatrist who can recommend treatment options to prevent the condition from worsening.
If you are suffering from bunions, contact Barbara J. Aung, DPM of Aung Foot Health Clinic . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
A bunion is formed of swollen tissue or an enlargement of boney growth, usually located at the base joint of the toe that connects to the foot. The swelling occurs due to the bones in the big toe shifting inward, which impacts the other toes of the foot. This causes the area around the base of the big toe to become inflamed and painful.
Why Do Bunions Form?
Genetics – Susceptibility to bunions are often hereditary
Stress on the feet – Poorly fitted and uncomfortable footwear that places stress on feet, such as heels, can worsen existing bunions
How Are Bunions Diagnosed?
Doctors often perform two tests – blood tests and x-rays – when trying to diagnose bunions, especially in the early stages of development. Blood tests help determine if the foot pain is being caused by something else, such as arthritis, while x-rays provide a clear picture of your bone structure to your doctor.
How Are Bunions Treated?
- Refrain from wearing heels or similar shoes that cause discomfort
- Select wider shoes that can provide more comfort and reduce pain
- Anti-inflammatory and pain management drugs
- Orthotics or foot inserts
- Surgery
If you have any questions, please feel free to contact our office located in Tuscon, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is an enlargement of the base joint of the toe that connects to the foot, often formed from a bony growth or a patch of swollen tissues. It is caused by the inward shifting of the bones in the big toe, toward the other toes of the foot. This shift can cause a serious amount of pain and discomfort. The area around the big toe can become inflamed, red, and painful.
Bunions are most commonly formed in people who are already genetically predisposed to them or other kinds of bone displacements. Existing bunions can be worsened by wearing improperly fitting shoes. Trying to cram your feet into high heels or running or walking in a way that causes too much stress on the feet can exacerbate bunion development. High heels not only push the big toe inward, but shift one's body weight and center of gravity towards the edge of the feet and toes, expediting bone displacement.
A podiatrist knowledgeable in foot structure and biomechanics will be able to quickly diagnose bunions. Bunions must be distinguished from gout or arthritic conditions, so blood tests may be necessary. The podiatrist may order a radiological exam to provide an image of the bone structure. If the x-ray demonstrates an enlargement of the joint near the base of the toe and a shifting toward the smaller toes, this is indicative of a bunion.
Wearing wider shoes can reduce pressure on the bunion and minimize pain, and high heeled shoes should be eliminated for a period of time. This may be enough to eliminate the pain associated with bunions; however, if pain persists, anti-inflammatory drugs may be prescribed. Severe pain may require an injection of steroids near the bunion. Orthotics for shoes may be prescribed which, by altering the pressure on the foot, can be helpful in reducing pain. These do not correct the problem; but by eliminating the pain, they can provide relief.
For cases that do not respond to these methods of treatment, surgery can be done to reposition the toe. A surgeon may do this by taking out a section of bone or by rearranging the ligaments and tendons in the toe to help keep it properly aligned. It may be necessary even after surgery to wear more comfortable shoes that avoid placing pressure on the toe, as the big toe may move back to its former orientation toward the smaller toes.
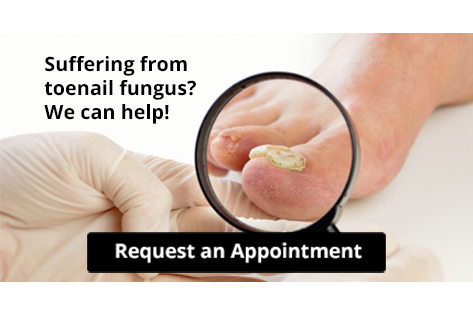
Need for Toenail Fungus Treatment

Yellowed, brittle, and unusual-looking toenails may indicate a fungal nail infection, known as onychomycosis. Experts caution that these infections persist without intervention and can easily be transmitted from person to person. These types of infections can be contracted through close contact or from barefoot walking in communal areas like locker rooms. The fungus infiltrates toenails, thriving in moist, sweaty footwear. Toenail fungus affects roughly one in ten people globally, and is more prevalent with age, affecting over half of individuals aged 70 and older. People who have diabetes or compromised immune systems are particularly vulnerable. If you notice a change in your toenails, it is suggested that you schedule an appointment with a podiatrist for an evaluation, diagnosis, and treatment.
If left untreated, toenail fungus may spread to other toenails, skin, or even fingernails. If you suspect you have toenail fungus it is important to seek treatment right away. For more information about treatment, contact Barbara J. Aung, DPM of Aung Foot Health Clinic . Our doctor can provide the care you need to keep you pain-free and on your feet.
Symptoms
- Warped or oddly shaped nails
- Yellowish nails
- Loose/separated nail
- Buildup of bits and pieces of nail fragments under the nail
- Brittle, broken, thickened nail
Treatment
If self-care strategies and over-the-counter medications does not help your fungus, your podiatrist may give you a prescription drug instead. Even if you find relief from your toenail fungus symptoms, you may experience a repeat infection in the future.
Prevention
In order to prevent getting toenail fungus in the future, you should always make sure to wash your feet with soap and water. After washing, it is important to dry your feet thoroughly especially in between the toes. When trimming your toenails, be sure to trim straight across instead of in a rounded shape. It is crucial not to cover up discolored nails with nail polish because that will prevent your nail from being able to “breathe”.
In some cases, surgical procedure may be needed to remove the toenail fungus. Consult with your podiatrist about the best treatment options for your case of toenail fungus.
If you have any questions, please feel free to contact our office located in Tuscon, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
Orthotics Can Help in Plantar Fasciitis Treatment

Orthotics are a common treatment for plantar fasciitis, a condition causing persistent heel and foot pain. These shoe inserts provide support and alignment correction, relieving pressure on the plantar fascia. By redistributing weight and reducing strain on the foot's arch, orthotics can help to alleviate discomfort and promote healing. They are designed to address specific imbalances during walking or standing, improving overall foot mechanics. Studies have shown that orthotics can effectively reduce pain and improve function for individuals suffering from plantar fasciitis. Custom-made orthotics are particularly effective at offering tailored support for individual foot shapes and conditions. In addition to other treatments, such as stretching exercises and wearing proper footwear, orthotics can help in managing and alleviating plantar fasciitis symptoms. If you suffer from the discomfort of plantar fasciitis, it is suggested that you schedule an appointment with a podiatrist who can determine the most suitable treatment for you, including custom-made orthotics as an option.
If you are having discomfort in your feet and would like to try orthotics, contact Barbara J. Aung, DPM from Aung Foot Health Clinic . Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Tuscon, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot Orthotics
Orthotics are shoe inserts that are meant to correct an irregular walking gait or provide cushioning to the feet. Orthotics come in a variety of different models and sizes, including over-the-counter and customizable variants. Customizable orthotics can be shaped and contoured to fit inside a specific shoe and are typically prescribed through a podiatrist who specializes in customized footwear and orthotics design and management.
Orthotics are beneficial because they can help prevent injuries from occurring and provide cushioning to keep pain levels down to a minimum. They also allow for the correct positioning of the feet. Orthotics can act as shock absorbers to help remove pressure from the foot and ankle. Therefore, orthotics can make bodily movements, such as walking and running, become more comfortable as well as help prevent the development of certain foot conditions.
Orthotics alleviate pain and make the foot more comfortable by slightly altering the angle at which the foot strikes the ground surface, therefore controlling the movement of the foot and ankle. Orthotics come in different variants and can be made of various materials. To determine what type of orthotic is most suited to your feet and your needs, it is best to consult your podiatrist. He or she will be able to recommend a type of orthotic that can help improve your foot function or prescribe a custom orthotic to best fit your feet.
What to Expect During Ingrown Toenail Surgery
 Ingrown toenail surgery, also known as partial nail avulsion, is a common procedure performed to treat ingrown toenails. It is often used for more severe cases of ingrown toenails, which do not respond to other conservative healing methods. During the surgery, the podiatrist administers local anesthesia to numb the toe, ensuring the patient's comfort throughout the procedure. Next, the podiatrist carefully removes a portion of the affected toenail, including the ingrown edge or spike that is causing pain and inflammation. This process may involve using surgical instruments or specialized tools to precisely trim the nail. For recurrent or severe cases, the podiatrist may also apply a chemical solution or use a laser to destroy the nail matrix, the area the nail grows from, to prevent the ingrown portion of the nail from regrowing. Then the toe is thoroughly cleaned. A sterile dressing may be applied to promote healing. The entire procedure typically takes less than an hour, and patients can usually resume normal activities shortly afterward. If you have an ingrown toenail, it is suggested that you consult a podiatrist who can offer correct treatment options, which may include surgery.
Ingrown toenail surgery, also known as partial nail avulsion, is a common procedure performed to treat ingrown toenails. It is often used for more severe cases of ingrown toenails, which do not respond to other conservative healing methods. During the surgery, the podiatrist administers local anesthesia to numb the toe, ensuring the patient's comfort throughout the procedure. Next, the podiatrist carefully removes a portion of the affected toenail, including the ingrown edge or spike that is causing pain and inflammation. This process may involve using surgical instruments or specialized tools to precisely trim the nail. For recurrent or severe cases, the podiatrist may also apply a chemical solution or use a laser to destroy the nail matrix, the area the nail grows from, to prevent the ingrown portion of the nail from regrowing. Then the toe is thoroughly cleaned. A sterile dressing may be applied to promote healing. The entire procedure typically takes less than an hour, and patients can usually resume normal activities shortly afterward. If you have an ingrown toenail, it is suggested that you consult a podiatrist who can offer correct treatment options, which may include surgery.
Foot surgery is sometimes necessary to treat a foot ailment. To learn more, contact Barbara J. Aung, DPM of Aung Foot Health Clinic . Our doctor will assist you with all of your foot and ankle needs.
When Is Surgery Necessary?
Foot and ankle surgery is generally reserved for cases in which less invasive, conservative procedures have failed to alleviate the problem. Some of the cases in which surgery may be necessary include:
- Removing foot deformities like bunions and bone spurs
- Severe arthritis that has caused bone issues
- Cosmetic reconstruction
What Types of Surgery Are There?
The type of surgery you receive will depend on the nature of the problem you have. Some of the possible surgeries include:
- Bunionectomy for painful bunions
- Surgical fusion for realignment of bones
- Neuropathy decompression surgery to treat nerve damage
Benefits of Surgery
Although surgery is usually a last resort, it can provide more complete pain relief compared to non-surgical methods and may allow you to finally resume full activity.
Surgical techniques have also become increasingly sophisticated. Techniques like endoscopic surgery allow for smaller incisions and faster recovery times.
If you have any questions please feel free to contact our office located in Tuscon, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Foot and Ankle Surgery
When conservative, noninvasive methods prove ineffective, surgery may be selected as the next course of action for the treatment of your foot or ankle condition. A wide number of foot and ankle surgical procedures exist, and it is up to your podiatrist to determine which intervention will be most appropriate and helpful for your case. Some surgical procedures include bunion surgery, fusion, hammertoe surgery, heel spur surgery, metatarsal surgery, nail surgery, neuroma surgery, reconstructive surgery, skin surgery, and tendon surgery. Typically, surgery is turned to as a definitive way to alleviate excessive pain or discomfort and to return your foot to full mobility.
Regardless of the location on the body, all surgical procedures require preoperative testing and examination to ensure the surgery’s success and preferred outcome. A review of your medical history and medical conditions will take place, as will an evaluation of any current diseases, illnesses, allergies, and medications. Tests such as blood studies, urinalyses, EKG, X-rays, and blood flow studies may be ordered. Because the procedure involves the foot and/or ankle, the structures of your feet while walking may also be observed by your podiatrist.
Care post-surgery will depend on the type of surgical procedure performed. Typically, all postoperative care involves rest, ice, compression, and elevation. To improve and ensure a safe recovery, your foot and ankle surgeon may also employ the use of bandages, splints, surgical shoes, casts, crutches, or canes. He will also determine if and when you can bear weight. A timely and thorough recovery is a priority for both you and your podiatrist, and carefully following postoperative instructions can help achieve this.
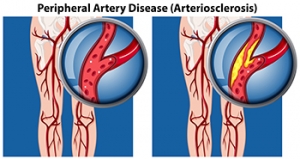
Walking and Peripheral Artery Disease
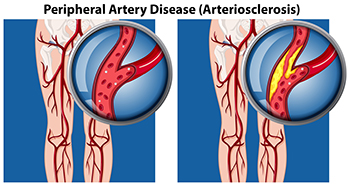
Peripheral artery disease, or PAD, can cause crampy, painful sensations in the legs during walking, often dismissed as mere exertion or aging. However, it is important not to overlook these symptoms, as PAD stems from fatty deposits that obstruct blood flow in the arteries outside the heart and brain. The lack of blood flow to the lower extremities can result in serious foot problems. Risk factors of peripheral artery disease include smoking, high cholesterol, high blood pressure, and diabetes. Classic PAD pain, known as claudication, typically occurs in the calf and subsides with rest. But other signs, like coldness, discoloration, or slow-healing sores in the feet may indicate inadequate blood supply, necessitating prompt treatment. Early detection via tests like the ankle-brachial index is vital, with lifestyle changes, such as quitting smoking, maintaining a healthy diet, and regular exercise, playing a key role in PAD management. Walking enhances blood flow in smaller leg arteries, creating alternative pathways to alleviate pain. Health experts recommend at least 30 minutes of walking, three times a week, for individuals with peripheral artery disease, to help slow the progression and associated complications. For help with the foot problems linked to PAD, it is suggested that you schedule an appointment with a podiatrist as quickly as possible.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Barbara J. Aung, DPM from Aung Foot Health Clinic . Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Tuscon, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.